Leaders
For decades it has been clear that when patients receive evidence-based care, their outcomes improve by 28-35% (Heater 1998).
In 2003, the Institute of Medicine called for 90% of healthcare decisions to be evidence-based by 2020 in order meet the goals set to achieve improved patient experiences and outcomes.
In 2009, Riley published 6 recommendations for achieving high reliability in healthcare organizations, which included a “culture of evidence-based practice”.
In 2010, Sammer et al., described the 7essential components of a culture of safety where EBP was one of the components.
In a study by Melnyk et al., (2012), clinicians identified current barriers to EBP; time to do EBP, EBP education and resources, availability of EBP mentors, organizational culture rooted in tradition, and resistance from clinical peers, colleagues, managers, and leaders. Clinicians expressed their need for support (as opposed to resistance) from the organization, managers, and interdisciplinary colleagues in order to be able to implement EBP.
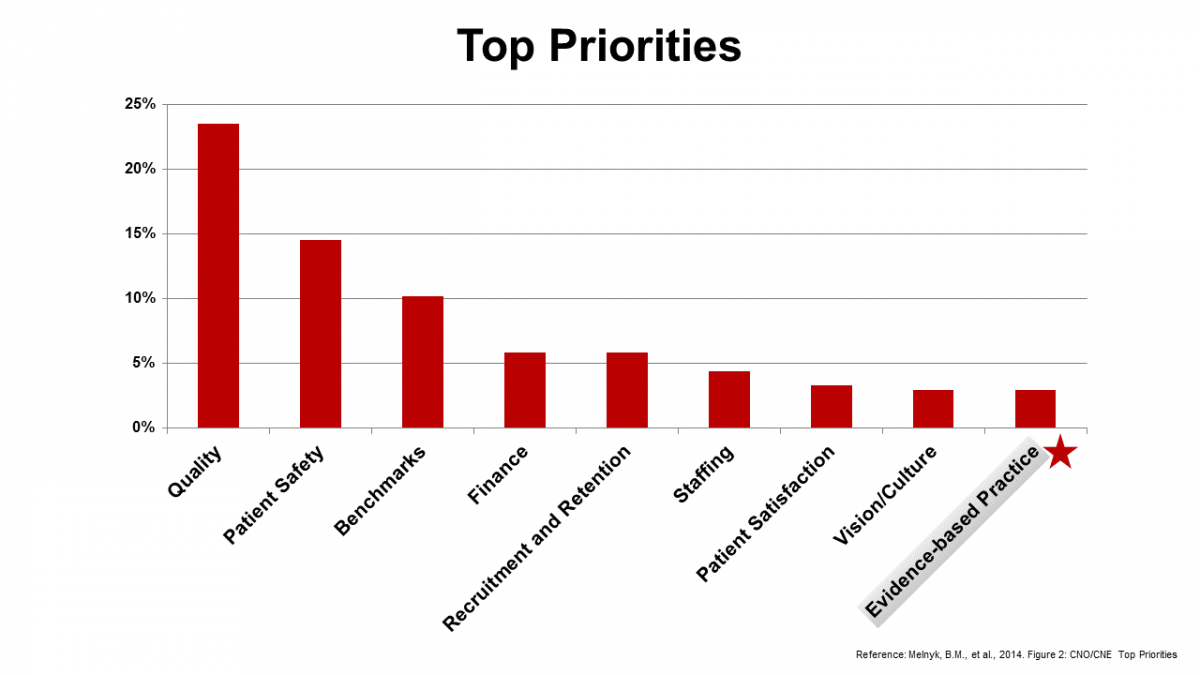
In 2014, Melnyk et al., surveyed chief nursing executives (CNE) related to evidence-based practice. The CNEs reported;
- Quality and safety were, overwhelmingly, their top 2 priorities
- 30 to 40% of hospitals were not meeting benchmarks for NDNQI performance metrics
- 20 to 30% of hospitals were above national benchmarks for core measures (e.g., falls, pressure ulcers)
- 90% believed that implementation of EBP reduced healthcare cost
- The large majority believed that EBP resulted in higher quality of care, safety and improved patient outcomes
However…
- 75% spent less than 10% of their budget on EBP
- EBP was listed as a very low priority!
- More than 50% reported that EBP was practiced “somewhat or “not at all” in their organization
- CNE’s personal beliefs in EBP were strong, but implementation of EBP in their own practice was low
- They reported having an inadequate number of EBP mentors in their organization to promote/sustain an EBP culture --------------------------------------------------------------------------------------------------
The case for EBP is clear and strong. It is the right thing to do. It drives best practice and best outcomes.
So, why is EBP not being implemented? Why is EBP such a low priority in healthcare organizations that are struggling to meet /exceed benchmarks and achieve excellence in patient outcomes? The disconnect is clear;
EBP is perceived as an additional outcome…that competes with the top priority outcomes of quality and safety.
Instead of;
EBP is the key strategy to implement…to achieve the top priority outcomes of quality and safety!
______________________________________________________
Despite the urgency to implement and sustain this new practice paradigm, the integration of evidence into practice continues to be perceived as a challenging and burdensome.
Much of the distress stems from a lack of EBP knowledge, skills and/or attitudes across the system, from executive suites to the bedside.
Healthcare leaders are responsible to address these challenges and be at the forefront of the paradigm shift.
Approaching the complex challenge to deliver best, evidence-based healthcare practices to achieve excellent outcomes will require innovative thinking and courageous acts.
The time is now.