The Fuld National Institute for EBP is a part of The Ohio State University College of Nursing. In a statement from College of Nursing’s Dean Karen Rose on June 20, 2024, “… we are starting a strategic process to reimagine our Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare. To this end, we are working on a Fuld 2.0 strategic plan and vision that will build upon the EBP expertise and programs within the CON. Although all the details of ‘Fuld 2.0’ are not yet fully developed and discussions continue to align around the way forward, I feel it is important to share that some previous revenue generating operations at the Fuld (i.e. immersions, etc.) will sunset at the end of the 2024 calendar year.”
All continuing education programs and events (5-day EBP Immersion, Leading EBP program, Practice + Process = Quality program, Teaching EBP program, Systematic review, Overcoming Barriers for Implementation program, Implementation. Facilitation Program, and all online modular programs) will sunset at close of business on December 20, 2024, 5pm EST. You have until this date and time, if not earlier per a registration date, to complete all requirements and download your CE certificate. You will not have access to any course after this date. Contact the College of Nursing Office of Continuing Education at NursingCE@osu.edu for lost certificates and questions after December 20, 2024.
In addition, the DNP Postdoctoral Fellowship, Fuld Funding Opportunities, Excellence in EBP and Outcomes in Healthcare Designation, and EBP National Summit will sunset on December 30, 2024.
Thank you for your partnership with the Fuld. We wish you all the best on your evidence-based journeys!
EBP Competencies
EBP Competencies for Practicing Registered Nurses and Advanced Practice Nurses in Real-World Clinical Settings are here!
Worldviews on Evidence-based Nursing; February 2014; Volume 11(1) The Establishment of Evidence-Based Practice Competencies for Practicing Registered Nurses and Advanced Practice Nurses in Real-World Clinical Settings: Proficiencies to Improve Healthcare Quality, Reliability, Patient Outcomes, and Costs
Bernadette Mazurek Melnyk, RN, PhD, CPNP/PMHNP, FNAP, FAANP, FAAN
Lynn Gallagher-Ford, RN, PhD, DPFNAP, NE-BC
Lisa English Long, RN, MSN, CNS
Ellen Fineout-Overholt, RN, PhD, FAAN
Background: Although it is widely known that evidence-based practice (EBP) improves healthcare quality, reliability, and patient outcomes as well as reduces variations in care and costs, it is still not the standard of care delivered by practicing clinicians across the globe. Adoption of specific EBP competencies for nurses and advanced practice nurses (APNs) who practice in real-world healthcare settings can assist institutions in achieving high-value, low-cost evidence-based health care.
Aim: The aim of this study was to develop a set of clear EBP competencies for both practicing registered nurses and APNs in clinical settings that can be used by healthcare institutions in their quest to achieve high performing systems that consistently implement and sustain EBP.
Methods: Seven national EBP leaders developed an initial set of competencies for practicing registered nurses and APNs through a consensus building process. Next, a Delphi survey was conducted with 80 EBP mentors across the United States to determine consensus and clarity around the competencies.
Findings: Two rounds of the Delphi survey resulted in total consensus by the EBP mentors, resulting in a final set of 13 competencies for practicing registered nurses and 11 additional competencies for APNs.
Incorporation of these competencies into healthcare system expectations, orientations, job descriptions, performance appraisals, and clinical ladder promotion processes could drive higher quality, reliability, and consistency of healthcare as well as reduce costs. Research is now needed to develop valid and reliable tools for assessing these competencies as well as linking them to clinician and patient outcomes.
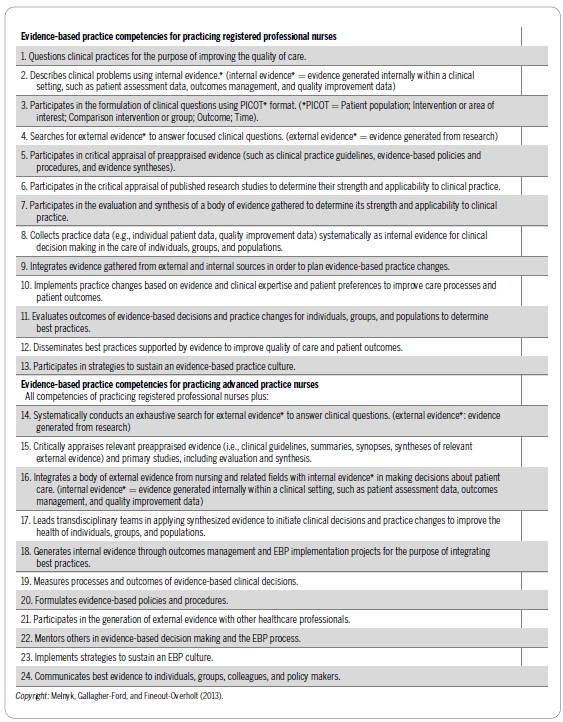
EBP Competencies are being integrated in different ways across both clinical and academic settings. Below are some examples:
- Clinical ladders
- Job descriptions and performance evaluations
- Leadership development course
- Onboarding program for new RNs
- Fellowship program for new Nurse Practitioners
- Interdisciplinary policy and procedure committee
- EBP Course rubric
If you are interested in integrating the EBP competencies in your organization, we have a measurement tool for your use. Click the contact button below for more information.